Public funding of homeopathy
Some people take the position that public money should not be spent on homeopathy because “it is a waste of tax-payers’ money”. Yet, very few people have access to the facts needed to weigh up this argument effectively.
Taking the UK’s National Health Service (NHS) as an example,
- In 2016, just £92,412 was spent on 40,000 homeopathy prescriptions from a total expenditure of £9.2 billion.1
- Out of the total NHS budget of £100 billion a year, roughly £4 million (0.004%) was spent annually on Homeopathy2 if you include everything from running the hospitals departments to paying the doctors.
- Five ‘observational studies’ tracked the outcome of patients being treated at NHS homeopathic hospitals. These studies consistently show that patients improve clinically following homeopathic treatment (often from chronic, difficult to treat conditions); some also highlight areas of potential economic benefit for the NHS as a whole in terms of reduced prescribing of conventional drugs (see below).
When considering value for money, it should also be remembered that if homeopathy patients were not treated with this service, they would have had to be offered other treatment options (if available), carrying their own associated costs.
Homeopathy should be considered in the same way as other NHS treatments
Some people argue that the NHS should not pay for homeopathy because we do not know that it works, whereas conventional medical drugs are ‘tried and tested’. Surprisingly this issue isn’t actually as clear-cut as one might think.
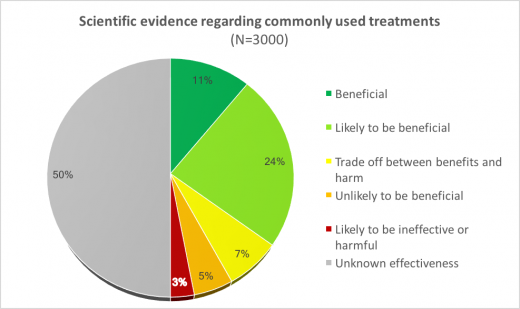
Analysis by the British Medical Journal’s (BMJ) Clinical Evidence3 shows that just 11% of 3,000 commonly used NHS treatments are known to be beneficial:
This data clearly indicates that the NHS pays for many treatments – besides homeopathy – for which the evidence is still unclear.
What evidence is there that homeopathy helps NHS patients?
The largest observational study at Bristol Homeopathic Hospital followed over 6,500 consecutive patients with over 23,000 attendances in a six-year period4. 70% of follow-up patients reported improved health; 50% reported major improvement.
More
The results of this 2005 Bristol study have been confirmed by a more recent observational study, published in 2016, involving an audit of just under 200 patients. The audit demonstrated that patients with long-term conditions who come under homeopathic care experience statistically significant improvements in their presenting symptoms and wellbeing.5
More
A 500-patient survey at the Royal London Homeopathic Hospital showed that many patients were able to reduce or stop conventional medication following homeopathic treatment.6
More
When assessing these clinical results, it is important to remember that NHS patients were usually referred for homeopathy because conventional medicine had failed to give satisfactory results, or conventional treatment was contra-indicated in their case. In 2016, NHS funding of homeopathy was stopped on the basis that it would save the NHS money. One has to ask, now that these homeopathy services are not available, who will treat these 1000s of patients instead? This raises serious ethical concerns about the removal of a service valued by patients, without provision of viable alternative treatments.
Removal of NHS funding for homeopathy – Key Points
- In July 2017 NHS England published draft guidelines advising local clinical commissioning groups to stop funding homeopathic prescriptions. The reason given was that there is no evidence of efficacy of homeopathic treatment – a claim supported by a single non-academic document – the 2010 Evidence Check 2 parliamentary report.
- During a 3-month Public Consultation on the draft guidelines, the HRI submission presented evidence demonstrating the clinical value of homeopathic prescriptions in the NHS, along with robust academic evidence of efficacy.
- HRI has received no response or explanation as to why this evidence and argumentation was insufficient justification for continuing homeopathic prescriptions on the NHS.
- After the Public Consultation had closed and no further input was possible, NHS England cited the Australian NHMRC report as additional justification for their decision. There was no opportunity for HRI to respond.
- In late 2017 the NHS Board met and agreed the draft guidelines with only minor alterations in response to the results of the Public Consultation. The recommendation to stop funding homeopathy prescriptions remained unchanged.
- In response, the British Homeopathic Association (BHA: a charity representing patients treated with homeopathy) challenged the decision in the High Court.
- Despite this legal challenge NHS England began removing funding for homeopathy in a number of locations, including the Royal London Hospital for Integrated Medicine, where the late Dr Peter Fisher – the Queen’s homeopathic physician – worked.
- The BHA’s legal case was heard over four days in May 2018 and examined whether NHS England had conducted their Public Consultation legally. In his opening statements, the presiding Judge Mr Justice Supperstone clarified that the court was unable to examine the issue of the scientific evidence base on Homeopathy.
- The court ruled that the Public Consultation had been conducted legally.
- By August 2018, funding for homeopathy on the NHS had completely stopped.
- NHS Digital, March 2017. Prescription cost analysis England 2016 | Link
- Freedom of Information Act request to the Department of Health by the Faculty of Homeopathy. Cost was £11.89 million between 2005 and 2008.
- BMJ Clinical Evidence, Efficacy Categorisations. 2017. Available from http://clinicalevidence.bmj.com/x/set/static/cms/efficacy-categorisations.html [Accessed 25 Sept 2017]
- Spence D, Thompson E A, Barron S J. Homeopathic treatment for chronic disease: a 6-year university-hospital outpatient observational study. J Altern Complement Med 2005; 5: 793-798 | PubMed
- Thompson E, Viksveen P, Barron S. A patient reported outcome measure in homeopathic clinical practice for long term conditions. Homeopathy, 2016; 105(4): 309-317 | PubMed
- Sharples F, van Haselen R, Fisher P. NHS patients’ perspective on complementary medicine. Complement Ther Med 2003; 11: 243-248 | PubMed